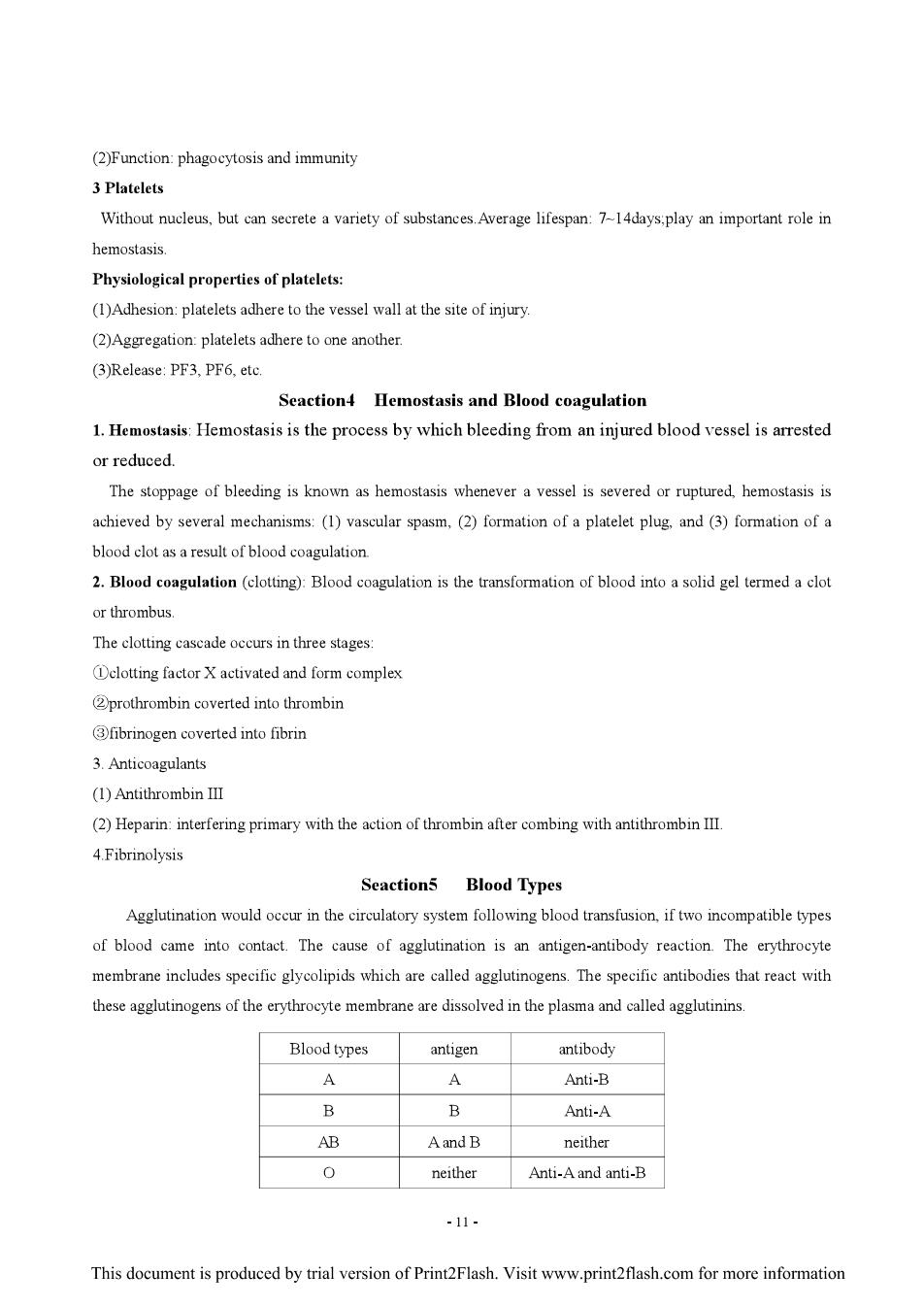
(2)Function:phagocytosis and immunity 3 Platelets Without nucleus,but can secrete a variety of substances.Average lifespan:7-14days;play an important role in hemostasis. Physiological properties of platelets: (1)Adhesion:platelets adhere to the vessel wall at the site of injury. (2)Aggregation:platelets adhere to one another. (3)Release:PF3,PF6,etc. Seaction4 Hemostasis and Blood coagulation 1.Hemostasis:Hemostasis is the process by which bleeding from an injured blood vessel is arrested or reduced. The stoppage of bleeding is known as hemostasis whenever a vessel is severed or ruptured,hemostasis is achieved by several mechanisms:(1)vascular spasm,(2)formation of a platelet plug,and(3)formation of a blood clot as a result of blood coagulation. 2.Blood coagulation (clotting):Blood coagulation is the transformation of blood into a solid gel termed a clot or thrombus The clotting cascade occurs in three stages: Dclotting factor X activated and form complex 2prothrombin coverted into thrombin 3fibrinogen coverted into fibrin 3.Anticoagulants (1)Antithrombin III (2)Heparin:interfering primary with the action of thrombin after combing with antithrombin III. 4.Fibrinolysis Seactions Blood Types Agglutination would occur in the circulatory system following blood transfusion,if two incompatible types of blood came into contact.The cause of agglutination is an antigen-antibody reaction.The erythrocyte membrane includes specific glycolipids which are called agglutinogens.The specific antibodies that react with these agglutinogens of the erythrocyte membrane are dissolved in the plasma and called agglutinins Blood types antigen antibody Y A Anti-B B B Anti-A AB Aand B neither 0 neither Anti-A and anti-B -11- This document is produced by trial version of Print2Flash.Visit www.print2flash.com for more information

Chapter 4 Circulation Teachering Hours 7 hours Intensive Teaching:Cardiac cycle:Bioelectrical phenomena and electrophysiological properties of cardiac muscle;Arterial Blood Pressure;Microcirculation;Neural regulation of Cardiovascular Activity Nodi for student:Bioelectrical phenomena of cardiac muscle;Factors affecting arterial pressure;Neural regulation of Cardiovascular Activity Seaction1 The Bump Function of Heart 1.Cardiac cycle The cardiac cycle includes two phases:systole and diastole,which forms into one mechanical activity cycle. Mechanical events during the cardiac cycle: (1)Atrial systole:bicuspid valve open;semilunar valve closed. (2)Ventricular systole: i)Period of isovolumic contraction:bicuspid valve closed;semilunar valve closed. ii)Period of rapid ejection:semilunar valve open:bicuspid valve closed iii)Period of slow ejection:semilunar valve open;bicuspid valve closed; (3)Ventricular diastole: i)Period of isovolumic relaxation:semilunar valve closed;bicuspid valve closed ii)Period of rapid filling:bicuspid valve open;semilunar valve closed iii)Period of reduced filling:bicuspid valve open:semilunar valve closed Heart sound:First heart sound:during ventricular systole:Second heart sound:during ventricular diastole 2.Cardiac output Stroke volume:stroke volume is referred to the volume ejected at each contraction by one side of the heart. Cardiac output:the volume ejected at each minute by one side of the heart. Cardiac output=stroke volumexheart rate Ejection fraction:The proportion of the end-diastolic volume that is ejected (i.e.stroke volume/end diastolic volume). Determinants of cardiac output (1)stroke volume:i)initial length(pre-load)-heterometric autoregulation ii)Contractility-homometric autoregulation iii)After-load (2)Effect of heart rate on cardiac output:Heart rate↑,cardiac output↑;Heart rate>2 00bpm,cardiac output↓ due to diastole too short,venous return too small. 3 Cardiac reserves The ability of cardiac output increasing with the strengthening of body metabolism is called cardiac reserve -12- This document is produced by trial version of Print2Flash.Visit www.print2flash.com for more information

Seaction2 Bioelectrical Phenomena of Myocardium 1.Cardiac Muscle Physiolgy 1.1 types of cardiomuscular cells (1)Autorhythmic cells:sinoatrial node;atrioventricular area:atrioventricular bundle;purkinje fiber (2)Unautorhymic cells:ventricular muscle;atrial muscle 1.2 Transmembrane Potential of Myocardial Cell and Their Ionic Basis 1.2.1 Resting Potential K+permeability↑,[K+]i>[K+loRP≌K+equilibrium potential 1.2.2 Action Potential (1)Phase 0(depolarization)Stimulation-partial depolarization-threshold potential (-70mV)-Na Channel opening -Na"influx into cell down electrochemical gradient -Vm less negative-0 mV-+30 mV(overshoot) (2)Phase 1:Intracellular potential rapidly recovers from+30mv to Omv ,the phase lasts about 10 ms. (3)Phase 2(plateau):the membrane potential keeps about Omv.lasts 100-150ms,which is the cause of the whole AP lasts a long period of time and The main difference between the AP of the myocardial contraction cell and that of a skeletal muscle fiber or a neuron is a lengthening of the AP Inward Ca2+current =outward K'current (4)Phase 3 (late repolarization):Character:the membrane potential repolarize quickly from Omv to -90mv. which lasts 100-150ms.There,is no distinct margin between phase 2 and phase 3. Mechanism:Phase 3 is the result of Ca2+current closing and increasing outward Kcurrent (5)Phase 4(resting stage):The membrane potential keeps around-90mv,but the exchange of ions continues Mechanism:During Phase 4.Na",Ca2efflux against concentration gradient:K+influx against concentration gradient to rebalance the concentration of ions outside and inside cell. 1.3 Electrical phenomena of automatic cells Spontaneous,phase 4 depolarization-the cause of automaticity pacemaker potential (1)Maximal repolarization potential at the end of phase 3. (2)Phase 4,depolarizes automatically (3)When depolarization reaches threshold level excitation(AP)appears. 2 Electrophysiological properties of cardiac muscle 2.1 Excitability Excitability index:1 threshold strength. Affecting factors: (a).RP level:the lower the RMP,the larger the distance from RMP to threshold potential,the larger the threshold strength needed to induce excitation-excitability,[K+lo (b)Threshold level: -13- This document is produced by trial version of Print2Flash.Visit www.print2flash.com for more information

Threshold level moves upward,the distance between it and RMP becomes larger,excitability decreases. (c)Behavior of Na+channel 2.2 Automaticity (Autorhythmicity) (1)Index of automaticity: frequency of discharge of pacemaker cell in S-Anode.100/min:dominant pacemaker A-V junction 50/min, Purkinje fiber 25/min Latent or subordinary pacemaker (2)Factors determining automaticity Frequency of excitation of pacemaker cell determinates the time for maximum diastolic potential to reach threshold potential. a.Rate of spontaneous,phase 4 depolarization.B receptor activation,If t HR b.Maximum diastolic potential level,gK+↑R↓ c.Threshold potential level 2.3 Conductivity 2.3.1.Index of conductivity-speed of conduction of AP 2.3.2.Factors determining conductivity of cardiac muscle a.Speed and amplitude of phase 0 depolarization (a)↑speed of phase0 depolarization→↑rate of generation of local current→↓time for depolarization to reach threshold potential -conductivity t (b)↑amplitude of phase0 depolarization→↑amplitude of local current→↑distance of depolarization of nearby membrane→↑conductivity.. (c)Speed and amplitude of phase 0 depolarization is determined by Vm More negative RP→↑speed of Na+-channel opening→↑speed of phase depolarization→↑speed of local current stimulation to reach to threshold potentialt speed of conduction b.↓excitability of nearby membrane area→↓conductivity Local current stimulus conducts to area which is in effective refractory period of premature potential.The stimulus can't induce a new AP and conduction block occurs. 2.4 Contractility 3 Electrocardiogram (ECG) The synchronized depolarizations spreading through the heart cause currents that establish field potential, whose differences can be amplified and detected by electrodes placed on the body surface.The record produced is called electrocardiogram A normal ECG is composed of P wave.QRS complex,and T wave.The P wave represents the depolarization process of both right and left atriums.The ORS complex is caused by the depolarization of both -14- This document is produced by trial version of Print2Flash.Visit www.print2flash.com for more information
ventricles and the T wave is generated by the repolarization process of the ventricles.The P-R interval is a measure of the time from the onset of atrial excitation to the onset of ventricular activation.The prolongation of P-R interval always indicates the disturbance in A-V conduction. Seaction3 Vascular Physiolgy 1 Functional properties of different blood vessels 1)Artery:Aorta and large artery:Pressure reservoir vessels 2)Capillary vessels:exchange vessels.Exchange of substances between blood and interstitial fluid 3)Venous Vessels,capacitance vessels:large vein,vena cava 2 Blood Pressure:the force exerted by the blood against any unit area of the vessel wall 2.1 Arterial Blood Pressure Systolic Pressure Diastolic Pressure Pulse Pressure MAP DP+1/3(pulse P) 2.2 Factors affecting arterial pressure (1)stoke volume (②)heart rate (3)peripheral resistance (4)aorta large artery (5)circulatory blood flow 2.3 Venous pressure and venous retum 2.3.1 Central venous pressure Affect factors:A Heart pump action B.Venous return velocity 2.3.2 Venous return and affecting factors A.Mean circulatory filling pressure B.Cardiac contractility C.Sympathetic nerve 3 Microcirculation,Interstitial fluid and Lymph 3.1 Microcirculation Microcirculation is the blood circulation between arteriole and veinule.The microcirculation is the place where the blood and interstitial fluid to carry out the exchange of substances. (1)Thoroughfare or preferential channel. (2)A-V anastomosis or A-v shunt. (3)Arteriole→metareriole→precapillary sphincter→true capillary→venule.. 3.2 Formation of interstitial fluid -15- This document is produced by trial version of Print2Flash.Visit www.print2flash.com for more information