。Diagnosis: NRDS-Surfactant deficiency ·Low lung volumes ·Air bronchograms Reticulo-granular pattern (ground-glass appearance) Cannot exclude infection as contributor
• Diagnosis: – NRDS-Surfactant deficiency • Low lung volumes • Air bronchograms • Reticulo-granular pattern (ground-glass appearance) – Cannot exclude infection as contributor
Actions: Given that symptoms are mild,oxygenation maintained,and blood gas acceptable,consider CPAP Pathophysiology is atelectasis ventilation/perfusion mismatch Maintain lung volumes with nasopharyngeal CPAP 4-6 cm H20 Monitor oxygenation,respiratory distress,intermittent blood gas Consider transfer if ventilation is not possible at the current institution
Actions: – Given that symptoms are mild, oxygenation maintained, and blood gas acceptable, consider CPAP • Pathophysiology is atelectasis → ventilation/perfusion mismatch • Maintain lung volumes with nasopharyngeal CPAP 4 – 6 cm H2O – Monitor oxygenation, respiratory distress, intermittent blood gas – Consider transfer if ventilation is not possible at the current institution
Over the next 2 hours,the infant develops marked intercostal indrawing,respiratory rate is 80 100 per minute,and breath sounds are decreased bilaterally. 0.70 oxygen is required to maintain saturations 89%. A repeat blood gas shows the following: Arterial blood gas in 0.70: pH 7.19 PaCO2 70 mm Hg Pa02 49 mm Hg HCO3 20 mmol What has happened? What is your next step?
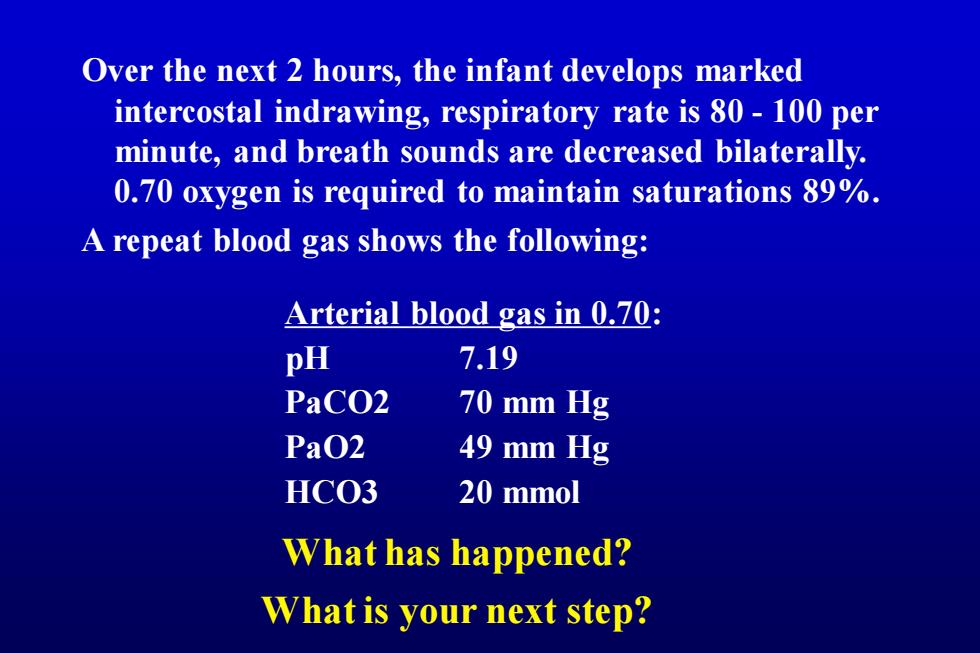
Over the next 2 hours, the infant develops marked intercostal indrawing, respiratory rate is 80 - 100 per minute, and breath sounds are decreased bilaterally. 0.70 oxygen is required to maintain saturations 89%. A repeat blood gas shows the following: What is your next step? Arterial blood gas in 0.70: pH 7.19 PaCO2 70 mm Hg PaO2 49 mm Hg HCO3 20 mmol What has happened?
。Assessment: Natural history of RDS is to worsen over the first 48 h Consider pneumothorax etc 。Actions: Transilluminate -Intubate 3.0 ETT Intubation criteria: Severe respiratory distress -PaC02>60 FiO2 in preterm infant>60% Diagnosis of moderate RDS with availability of surfactant Place umbilical arterial line
• Assessment: – Natural history of RDS is to worsen over the first 48 h – Consider pneumothorax etc • Actions: – Transilluminate – Intubate 3.0 ETT • Intubation criteria: – Severe respiratory distress – PaCO2 > 60 – FiO2 in preterm infant > 60% – Diagnosis of moderate RDS with availability of surfactant – Place umbilical arterial line
The infant is intubated uneventfully with a 3.0 ETT. He is receiving bag mask ventilation in 100%02 and has saturations of 99%. Several mechanical ventilators are available,including models with intermittent mandatory ventilation, patient triggered ventilation,and high frequency oscillatory ventilation. Which ventilator will you select? What ventilatory settings and parameters will you prescribe?
The infant is intubated uneventfully with a 3.0 ETT. He is receiving bag mask ventilation in 100% O2 and has saturations of 99%. Several mechanical ventilators are available, including models with intermittent mandatory ventilation, patient triggered ventilation, and high frequency oscillatory ventilation. What ventilatory settings and parameters will you prescribe? Which ventilator will you select?